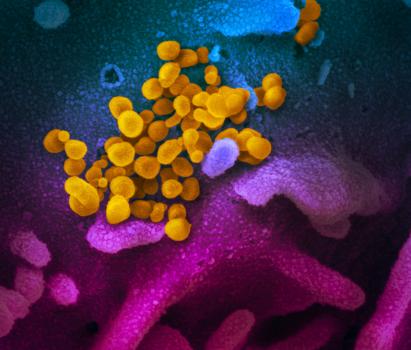
The Centers for Disease Control (CDC) has issued important information regarding the Coronavirus (COVID-19). The respiratory virus was first identified in 2019 and is has spread quickly across the globe.
According to the CDC, some people are at higher risk of getting very sick from this illness. This includes:
- Older adults
- People who have serious chronic medical conditions like:
- Heart disease
- Diabetes
- Lung disease
FACT SHEET: Know the facts about coronavirus disease 2019 (COVID-19) and help stop the spread of rumors.
CORONA VIRUS: What you need to know about the disease
WHAT TO DO IF YOU ARE SICK: If you are sick with the virus, or suspect you are, follow these steps provided by the CDC to help prevent spread of the virus.
SYMPTOMS of CORONAVIRUS: Patients with COVID-19 have mild to severe respiratory illness. Deaths have been reported.
Insurance carriers have responded and most are waiving the Copayment and Deductibles for testing. Blue Cross / Blue Shield of Texas, our states largest insurance provider released a statement today
| COVID-19 Coverage Information for Employers and Members We are closely monitoring the 2019 Novel Coronavirus (COVID-19) outbreak. We are committed to helping our employer customers and members stay informed and educated about COVID-19 and assisting those who might be affected. With regard to treatment for COVID-19, our plans cover medically necessary health benefits, including physician services, hospitalization and emergency services consistent with the terms of the member’s benefit plan. Members should always call the number on their ID card for answers to their specific benefit questions. For diagnostic testing for COVID-19, please note the following coverage information. Coverage for fully insured members: Effective immediately for all fully insured members, for testing to diagnose COVID-19 when medically necessary and consistent with Centers for Disease Control and Prevention (CDC) guidance: |
| · No prior authorization needed
· No member copays or deductibles The same coverage above applies to HSA qualified high-deductible health plans, pursuant to the IRS notice on COVID-19 issued March 11, 2020. Coverage for self-insured and split-funded* members: Self-insured and split-funded employers must opt in to offer their employees the testing to diagnose COVID-19 when medically necessary and consistent with CDC guidance with: |
| · No prior authorization needed
· No member copays or deductibles Action needed: Self-insured and split-funded groups must communicate their agreement to opt in by emailing their account executive or broker to activate this coverage. These groups must opt in by March 31, 2020.
|
We hope everyone takes care and gives special attention to those friends, family and loved ones that are considered Higher Risk. If you have questions about how you insurance is covering the testing and treatment, feel free to call us at 800-362-2809
